Discover the 2025 guide to Type 2 diabetes care updated treatments, lifestyle tips & diet plans to manage blood sugar and live healthier every day.
Introduction: You’re Not Alone in This
Living with Type 2 diabetes can be overwhelming at times we get it. This little bit of awareness induces you to consistent checks of sugar , alteration of diet planning, and soon , but the reality is that adequate proper knowledge with right care fosters tour life health and happily .
The comprehensive guidance explore you to access update options of treatment, life style changing guideline, and easy to follow up strategy which promote you to manage the diabetic very smoothly and more effective in 2025.
Let’s begin foe exploring the strategy for management.

What Exactly Is Type 2 Diabetes?
Think of Type 2 diabetes as a traffic jam in your body. The sugar (glucose) in your blood can’t get into your cells properly because insulin ,the hormone that helps sugar enter cells — isn’t working well. Your body either:
Can’t use insulin effectively (insulin resistance), or
Doesn’t produce enough insulin
The result? Too much sugar stays in your blood, which can cause long-term damage to your organs.
Who Is at Risk in Type 2 diabetes?
Type 2 diabetes can affect anyone, but some people are at higher risk:
* Over 40 years of age
* Overweight or obese
* Family history of diabetes
* Sedentary lifestyle
* High blood pressure or cholesterol
* Women with PCOS or gestational diabetes
**Example:**
Sunita, a 42-year-old schoolteacher, ignored her constant tiredness and thirst. A routine blood test revealed high blood sugar levels. With small diet changes and a morning walk routine, she turned her health around in 6 months.

Whom to screen of Type 2 diabetes ? (in absence of symptoms)
- Age ≥30 years, in absence of risk factors
- All overweight or obese adults (BMI ≥23 kg/m2), with one or more risk factors [first degree relatives with T2D, H/O CVD, HTN, Dyslipidemia (HDL<35 mg/dl, TG>250 mg/dl), PCOS]
In case of children older than 10 years: BMI>85th centile with one risk factor (maternal H/O GDM, family H/O T2D, dyslipidemia, HTN, PCOS
- Patients with prediabetes (A1C ≥5.7% , IGT, or IFG) should be tested yearly
- Women who were diagnosed with GDM should have lifelong testing at least every 1-3 years
Screening frequency of Type 2 diabetes :
- Repeat testing every 3 years if normal
- More frequent testing based on risk profile and results
- Criteria for screening and diagnosis
| Prediabetes | Diabetes | |
| Fasting plasma glucose | 100-125 mg/dl | ≥ 126 mg/dl |
| 2hr post 75 gm Glucose load plasma glucose | 100-125 mg/dl | ≥ 200 mg/dl |
| HbA1c | 5.7-6.4 % | ≥ 6.5 % |
| Random plasma glucose | ≥ 200 mg/dl |
Goals of Therapy of Type 2 diabetes:
- Alleviate symptoms
- Prevent acute and chronic complications
- Improve quality of life
Screen for co-morbidities & complications of Type 2 diabetes
| What to screen for | How to screen | Frequency |
| Hypertension | Blood Pressure | Every follow up visit |
| Dyslipidemia | Fasting lipid profile( preferably after glycemic control) | Annually |
| Cardiovascular | ECG | Annually |
| Retinopathy | Dilated Fundus examination/Fundus photography | Annually |
| Neuropathy | Pinprick sensation10-g monofilamentVibration perception threshold | Annually |
| Peripheral arterial diseases | Distal pulses+_ ABI | Annually |
| MASLD | FIB4( Age, SGPT, SGOT, Platelet count) | Annually |
| Vit B12 | If on Metformin for more than5years | Annually |
| Psychosocial | Assessment of depression , anxiety, diabetes distress | Annually |
ABI: Ankle Brachial ( systolic BP) Index , after age of 50 years or, with risk factors like CAD

Signs & Symptoms to Watch Out For Type 2 diabetes:
Type 2 diabetes often develops slowly, and many people don’t notice symptoms early on. But common signs include:
* Constant thirst and hunger
* Frequent urination
* Fatigue
* Blurred vision
* Slow healing of wounds
* Tingling in hands and feet
* Sudden weight loss
If you notice any of these, **get your blood sugar checked**. Early detection makes a huge difference.

Updated Treatment Options in 2025 of Type 2 diabetes
The good news? Treatment has come a long way. It’s no longer just about pills and insulin. The focus is now on **personalized care** based on your body, health conditions, and lifestyle.
Whom to treat of Type 2 diabetes ?
- All patients with diabetes not responding to lifestyle therapy for a period of 3 months should be started on pharmacological therapy
- If initial HbA1c ≥ 7.5%, pharmacological treatment should be started along with lifestyle changes
Which drug to choose in Type 2 diabetes case?
Oral antidiabetic drugs
1st Line Agent
Metformin is recommended as the first line treatment for all patients with type 2 diabetes mellitus unless not tolerated or contraindicated
Contraindications in Type 2 diabetes :
- eGFR<30ml/min/1.73m2),
- lactic acidosis,
- any acute illness or,
- hypoxaemic states
2nd Line Agent
- Add Dapagliflozin to Metformin if blood glucose is not controlled with Metformin alone
- Avoid Dapagliflozin if
- Active/ recurrent genitourinary infectionsKetoacidosisSevere dehydrationDocumented end stage renal diseaseOn hemodialysis
- If Dapagliflozin is contraindicated, start Linagliptin
3rd Line Agent (to be decided by specialist)
| DRUG | INDICATIONS | CAUTION |
| Linagliptin | If not already added | History of acute pancreatitis Hyper sensitivity on previous exposure |
| Dapagliflozin | If not already added | Recurrent genitourinary track infection, H/O upper urinary tract infections, severe dehydration, severely insulinopenic |
4th Line Agent
- Glimepiride: 1 mg OD / BD, intensify up to 4 mg BD
- Risk of hypoglycemia, weight gain
- Other agents if needed
- Pioglitazone 15 mg OD (caution in heart failure, oedema)
- Voglibose 0.3 mg OD with meals up to three times a day (GI side effects)
Doses of Oral Anti-hyperglycemic agents of Type 2 diabetes
| DRUG | INITIAL DOSE | MAXIMUM DOSE | FREQUENCY OF DOSE |
| Metformin | 500 mg to 1 gm | 2.5 gm | OD, BID, TID |
| Sulphonylureas Glimepiride | 1 to 4 mg | 8 mg | OD, BID |
| Linagliptin | 5 mg | 5 mg | OD |
| AGI Voglibose | 0.2 mg with each meal | 0.3 mg with each meal | With meals |
| Pioglitazone | 15 mg | 30 mg | OD |
| Dapagliflozin | 5-10 mg | 10 mg | OD |
Insulin (specialist initiation) for Type 2 diabetes :
- Indications of Insulin
- Catabolic state/ uncontrolled hyperglycemia
- Major surgery/ acute metabolic/ infective complications
- Preconception and pregnancy
- Consider insulin if at the time of diagnosis, patient is symptomatic and have one of the following: Fasting plasma glucose > 250mg/dl or Postprandial glucose > 300mg/dl or HbA1c >10%
- Insulin can be considered at any stage in type 2 diabetes mellitus. However, it is recommended to consider insulin after failure of 3 oral antidiabetic drugs
Which insulin to initiate for Type 2 diabetes ?
- If fasting blood glucose is predominantly raised – consider Basal insulin
- If postprandial blood glucose is predominantly raised – consider premixed insulin or basal-bolus regimen
- Human insulins are generally preferred over analog insulins, especially because of price advantage
- SMBG (Self Monitoring of Blood Glucose) to be strongly encouraged, whenever insulin is initiated
How to initiate insulin for Type 2 diabetes :
- Basal insulin: 0.1 -0.2 units/ kg/ day or, 10Units/day; generally, at a fixed time at night
Titrate every 3rd day after monitoring FPG
- Pre-mixed insulin: 0.4-0.5 units/ kg/ day; administer 2/3rd of the total daily dose with morning meal and 1/3rd with evening meal
[Analogue pre-mixed insulin: to be injected within 10 min of onset of meal, while human pre-mixed insulin needs to be injected about 30 min pre-meal]
- For Basal bolus: 50% dose as basal, rest 50% in three divided doses as prandial insulin
Glycemic goals for most of Type 2 diabetes patients
| Fasting Plasma Glucose | 80-130 mg/ dl |
| Postprandial Plasma Glucose | <140-150 mg/ dl |
| HbA1c | <7% |
Postprandial glucose measurements should be made 2 h after the beginning of the usual meal (and not glucose load). Usual medicines should also be taken
Non-glycemic goals of Type 2 diabetes
| Nonglycemic goals | |||
| Blood pressure | |||
| Higher cardiovascular or,renal risk | <130/80mmHg | ||
| Low cardiovascular risk | <140/90mmHg | ||
| Lipid | |||
| High risk | Very High risk | Extremely high risk*** | |
| LDL-(mg/dl) | <100 | <70 | <55 |
| Non HDL-C(mg/dL) | <130 | <100 | <80 |
| TG(mg/dL) | <150 | <150 | <150 |
| Antiplatelet agent | Use aspirin as secondary prevention stage (75 – 150 mg/dL) Clopidogrel for those with aspirin allergy /intolerance Aspirin is the primary prevention :only in those with very high risk , after discussion with patients regarding possible benefits vs risk of bleeding | ||
| Follow-up |
Physical examination of Type 2 diabetes
| Baseline | Follow up | |
| Physical examination | ||
| Height, weight and BMI (try to achieve ideal body weight) | ü | Every visit |
| Blood pressure | ü | Every visit |
| Fundoscopic examination (refer to eye specialist) | ü | Every year if no retinopathy |
| Skin examination (e.g., insulin injection sites, lipodystrophy) | ü | Every visit |
| Comprehensive Foot examination Visual inspection (e.g., skin integrity, callus formation, foot deformity or ulcer, toenails) Determination of pinprick sensation, 10g monofilament examination, vibration perception and temperature sensation Screen for Peripheral Arterial Disease – pedal pulses (age>50 years or risk factors like CAD) | ü | Atleast annually |

Laboratory investigations of Type 2 diabetes
| Investigations | ||
| Fasting and 2-hour postprandial glucose | ü | At least every 3months |
| HbA1c | ü | At least 6 monthly |
| Fasting lipid profile | ü | At least annually |
| Serum creatinine & eGFR | ü | At least annually; if favorable profile, every 2-3 years |
| Urinalysis(including microscopy and urine microalbumin screening) | ü | At least annually |
| Liver function tests, platelet count | ü | At least annually |
| ECG | ü | Annually |
Criteria for referral
- Diabetes in young (<25 years)
- Where the type of diabetes is in question
- Diabetes associated with significant comorbidities
- In the presence of acute metabolic complications of diabetes
- Uncontrolled hyperglycemia even after following standard treatment care
- Chronic complications of diabetes demanding specialized care
- Diabetes with severe infections and/or foot ulcers
- Morbid obesity
- Initiation of insulin
Special situation: Gestational Diabetes
Pre-pregnancy counseling
Pre pregnancy counselling:
Universal screening of all women of reproductive age group, planning pregnancy for hyperglycemia
Effective contraception until glycemic status, HTN, weight optimized
Comprehensive nutrition assessment (meal planning, correction of dietary nutritional deficiency), regular moderate exercise, adequate sleep
Encourage weight loss in individuals with overweight
Co-morbidity screening in women with pre existing diabetes (retinopathy screening, lipid profile, TSH, ECG, serum creatinine and urine ACR)
Switch to insulin and stop all OHA (except metformin)
ACEI/ARB/Statins should be stopped prior to conception.
Diagnosis and management:
Diagnosis and management:
Universal screening for all pregnant women with one step 2 hours OGTT with 75 g anhydrous glucose (irrespective of fasting or, non-fasting state) at 15 antenatal contact (preferably in first trimester)
If first test is negative, then repeat test to be done at 24-28 weeks of gestation
2 hours OGTT cut off 140 mg/dl is taken as diagnostic of GDM
If pre pregnancy glycemic status is not documented, screen all pregnant women with FBG, PPBG, and HbA1c at first visit
Start lifestyle modification after diagnosis of GDM is established
Follow up with FBG, PPBG after 2 weeks
If treatment goal (Table 1) not achieved, start insulin
Goals of treatment
| Table1: Treatment Goals | |
| Value | Target(mg/dl) |
| FPG | <95 |
| 2hr PPPG | <120 |
- Premixed insulin( 30:70) S/C30 minutes once a day before breakfast
- If FBG is above target level, also start pre dinner insulin
- 120-160 mg/dl:4units
- 160-200 mg/dl:6units
- >200mg/dl:8units
Insulin dose adjustments
Monitor with FBG and 2 hours PPBG every 3rd day
Insulin dose adjustment
| FBG | PPBG | Insulin dose |
| <95 mg/ dl | <120 mg/dl | Continue previous dose |
| <95 mg/ dl | >120 mg/dl | Increase per breakfast dose by 2 units |
| >95 mg/ dl | <120 mg/dl | Increase dinner dose , continue same dose per breakfast |
| >95 mg/ dl | >120 mg/dl | Increase 2 units per dinner dose, increase per breakfast dose by 2 units |

Referral criteria
- Vomiting and not able to take food orally
- Fasting blood glucose.200mg/dl or,PPBG >250 mg/dl with or, without mitformin or, insulin treatment
- Total daily dose of insulin exceeds 20 units
- Frequent hypoglycemic episodes more than once a day .
Metformin:
It reduces glucose production in the liver. Doctors still prescribe this first because it’s effective and safe.
Encourage regular SMBG/ glycemic monitoring
Metformin :
- Can be considered after 20 weeks of pregnancy (maximum dose 2gm/day) after discussing risk vs benefits with patient.
- Metformin not to be used in presence of HTN, preeclampsia
- If not controlled with MFB, add insulin ( if not started earlier )
Antenatal care
- Fetal anomaly scan at 18-20 weeks and fetal growth scan at 28-30 weeks
- Low dose Aspirin (75 mg) starting at 12-16 weeks in high-risk cases of GDM (chronic hypertension or, an auto immune disease, or presence of multiple risk factors like nulliparous, obesity, age > 35years)
- HTN-To be monitored at each visit.
Blood pressure threshold of 140/90 mmHg for initiation or titration of antihypertensive therapy
- If antenatal dexamethasone injection is given for fetal lung maturation in case of early delivery, modify Insulin dose according to CBG during this period
Labour and delivery
- Induction of labour at or after 39 weeks if not delivered spontaneously.
- LSCS for fetal macrosomia (>4 kg)
- To monitor CBG frequently
- Insulin infusion to be initiated according to CBG values
Postpartum management
Postpartum, insulin requirements will reduce significantly Closely monitor the glycemic status and adjust
therapy accordingly
Initiate early breast feeding
CBG monitoring of new born within first hour of birth and repeated & hourly up to 4 normal readings (risk of hypoglycemia)
OGTT to be performed at 6 weeks postpartum and high risk of future diabetes in mother and offspring to
be discussed
If negative (2 hrs OGTT <140 mg/di), then annual screening
New-Gen Medications You Should Know:
GLP-1 Receptor Agonists (e.g., Semaglutide, Liraglutide)
* Help you feel full and eat less
* Aid weight loss
* Protect the heart
* Taken weekly or daily by injection
SGLT2 Inhibitors (e.g., Dapagliflozin, Empagliflozin)
* Help kidneys flush out excess sugar through urine
* Lower heart failure and kidney risk
* Also help with weight control
**Example:**
Amit, 50, had diabetes and heart issues. His doctor prescribed an SGLT2 inhibitor. Within 3 months, his sugar levels stabilized, and his blood pressure improved.
Combination Therapies
Doctors now often combine medications (oral + injection) based on your overall health. This gives better control with fewer side effects.
Your Diet Plan: No Starving, Just Smart Eating
You don’t need to give up your favorite foods completely — just **make smarter choices**.
Focus On:
Whole grains (oats, brown rice)
High fiber veggies (carrot, spinach, beans)
Lean protein (dal, tofu, eggs, chicken)
Healthy fats (nuts, seeds, olive oil)
Low glycemic index (GI) foods
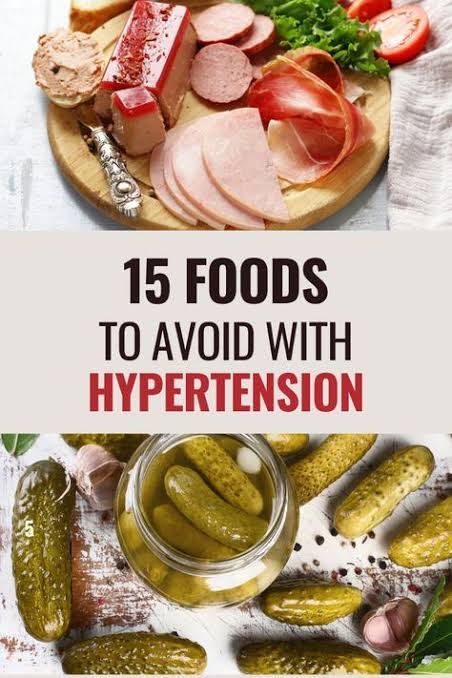
Avoid or Limit:
* White rice, white bread
* Sugary drinks and snacks
* Packaged juices
Simple Tip:
Use a small plate and fill half with veggies, one-quarter with protein, and one-quarter with grains.
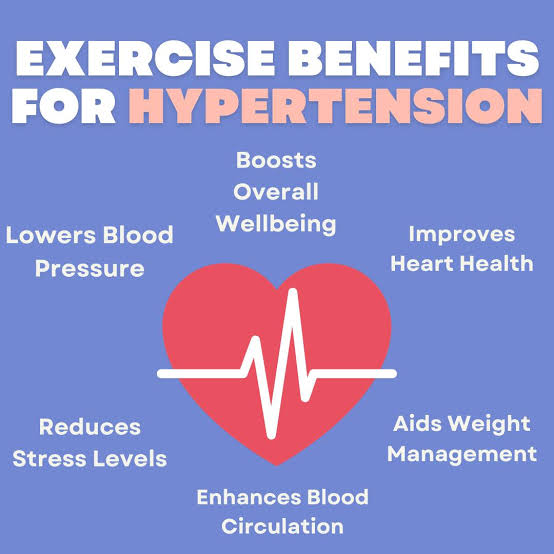
Lifestyle: Small Steps, Big Changes basically avoided sedentary lifestyle
Move More
Just 30 minutes of daily activity can lower blood sugar and improve mood.
Ideas:
* Brisk walking
* Cycling
* Yoga
* Dancing
Even 10-minute post-meal walks can reduce sugar spikes.
Prioritize Sleep:
Sleep impacts your sugar. Aim for 7–8 hours of sleep each night. Create a routine — lights off by 10:30 PM, avoid screens 1 hour before bed.
Stress Less
Chronic stress increases cortisol, which spikes your blood sugar. Try:
* Deep breathing
* Meditation
* Music therapy
* Talking to a friend or therapist
Modern Tools for Better Management:
Advise lifestyle modifications:
- Nutrition
- Physical activity
- Adequate Sleep
- Tobacco avoidance
- Moderation of alcohol intake
Nutrition
- Calorie restriction (if BMI is increased)
- Balanced diet
- Adequate fruits & vegetables
- Avoid deep fried foods, soft drinks, processed foods
Physical activity
- 150 min/week moderate exertion,
- spread over at least 3 days/week,
- with no more than 2 consecutive days without activity
- ± Resistance exercise
- ± Balanced exercise for elderly
Tobacco avoidance
- No tobacco products
Moderation of alcohol intake
- No more than 1 drink per day for adult women
- No more than 2 drinks per day for adult men
Continuous Glucose Monitors (CGMs)
Wearable devices that track sugar 24/7. Great for understanding how your body reacts to food, exercise, or sleep.
Diabetes Apps
Apps like
mySugr
Healthifyme
BlueLoop
All above mention Apps help track your sugar, food, meds, and exercise.
Smart Watches
Many now sync with CGMs or health apps to alert you if sugar levels go too high or low.
Managing Complications Early
Type 2 diabetes, if left uncontrolled, can lead to:
* Heart disease
* Kidney problems
* Vision loss
* Nerve damage
* Foot ulcers
To prevent this:
* Monitor sugar regularly
* Get annual **eye**, **foot**, and **kidney** check-ups
* Control BP and cholesterol
* Stay active and eat healthy
Is Reversal Possible?
Absolutely Yes, in some early cases, diabetes can be reversed through:
Major weight loss
Regular exercise
Strict low-carb diet
This is called diabetes remission ,sugar levels stay normal without medication.
Example:
Neha, 35, lost 12 kg over a year, followed a low-GI diet, and walked daily. Her doctor confirmed her sugar levels were now in the normal range without meds.
When to Visit Your Doctor
Regular follow-ups are key. Don’t wait till problems show up.
Visit your doctor if you notice:
* Vision changes
* Foot pain or wounds
* Frequent infections
* Tingling or numbness in hands/feet
* Sudden weight loss
Get your **HbA1c test every 3–6 months** to track long-term sugar control.
For Older Adults with Type 2 Diabetes
If you’re over 60, managing diabetes needs extra care:
Choose easy-to-follow routines:
* Avoid risky low sugar episodes
* Focus on heart and bone health
* Discuss meds that suit your age and kidney function
Summary Checklist: Your Daily Routine
| Habit | Why it matters |
| Eat balanced meals | Stabilizes sugar throughout the day |
| Walk 30 mins | Boosts insulin sensitivity |
| Take meds on time | Keeps sugar in range |
| Relax daily | Reduces stress hormones |
| Stay hydrated | Helps flush excess sugar |
| Monitor sugar | Early detection of highs/lows |
Real-Life Meal Plan Example:
In Breakfast: 2 boiled eggs + 1 slice multigrain toast + green tea
In Mid-morning: Handful of nuts or a fruit (apple)
At Lunch:Brown rice + dal + mixed veg + salad
In Evening Snack: Roasted chana or sprouts
In Dinner: Grilled paneer/tofu + soup + 1 small roti
At Before Bed: Warm turmeric milk (no sugar)
Final Words: You’ve Got This!
Managing Type 2 diabetes doesn’t mean giving up joy. It means being aware, making mindful choices, and celebrating small wins.
Take it one step at a time. Don’t aim for perfection — aim for **progress**.
Remember, every healthy choice you make is a step toward a longer, better life.
You’re not alone — and you’ve got what it takes.
Type 2 Diabetes in Adolescents: Why Awareness Matters
Children and adolescents now constitute about a third of the world’s total population and nearly half of the population of developing countries. Numbering over 1 billion worldwide, today’s adolescent is the largest cohort ever to transition into adulthood.
Unfortunately, there is a common misconception that NCDs do not affect adolescents; however, NCDs and risk factors have an enormous impact on the health of adolescents.
Adolescents are often targeted by the companies advertising food, tobacco, or alcohol, and many grow up in environments that are not conducive to them adopting healthy lifestyles (e.g., parental use of tobacco and alcohol and peer pressure). Many health-related behaviors usually stated in the adolescent phase, like becoming obese, physical inactivity, overeating, excess use of sugar (chocolate and cold drinks), and fat, are responsible key factors for about 40% of non-communicable diseases, especially type 2 diabetes.
So, awareness about type-2 diabetes among the adolescent population is a very crucial issue today because of the enhancement of the prevalence of this particular disease in the younger generation, which has the potential for long-term complications, and preventing or delaying the onset of the disease through lifestyle modifications.
1. Rising Prevalence:
Diseases like type- 2 diabetes are becoming very challenging and threatening for the health of children and adolescents today, and also trends were not seen previously. This shifting of advancement is found among more young people in earlier life in a complicated form.
2. Increased Risk of Complications:
Type -2 diabetes has the ability to promote the making of serious long-term complications likely cardiovascular disease, kidney disease, eye damage (retinopathy), and nerve damage (neuropathy). These complications become more curious for those who are affected in the adolescent stage rather than in late adulthood.
3. Potential for Prevention and Delay:
Most of the cases are preventable through changing their sedentary lifestyle, likely adopting a healthy diet intake, regular physical exercise, and regular monitoring of BMI. Awareness fosters empowerment for adolescents to make informed choices for reducing high risk.
4. Managing Existing Diabetes:
For an adolescent who has already been diagnosed as living with type -2 diabetes, awareness is the best tool for proper management, including blood sugar control, adherence with medication, and proper monitoring.
After all, it is the essence of the diseases; raising awareness is the crucial factor for their prevention, early detection, effective management, and overall public health wellness.
Disclaimer:
This content has not any intention to misconduct any steps of treatment guidance towards the type -2 diabetes patients; all the data and treatment protocol has been explored according to different medical professionals, but it is the recommendation to all the audience to follow the medical advice from your medical practitioner accordingly, because your degree of disease is very specific.
Quick FAQs
Q. Can I eat sweets at all?**
Yes, occasionally — just plan them into your meals and monitor sugar after.
Q. Is walking enough exercise?**
Yes, brisk walking daily helps. Combine with stretching or light strength training for best results.
Q. Can diabetes be reversed naturally?**
In early stages, yes — with weight loss and lifestyle changes under medical supervision.
Q. Is walking enough exercise?**
Yes, brisk walking daily helps. Combine with stretching or light strength training for best results
Q. Can diabetes be reversed naturally?**
In early stages, yes — with weight loss and lifestyle changes under medical supervision.
Q. Is brown sugar or jaggery better than white sugar?**
Not really. They still affect blood sugar. Use all sweeteners in moderation.
Q. Is Type 2 diabetes genetic?**
Yes, genetics play a role — but lifestyle is a bigger factor.
Q. Can I eat sweets occasionally?**
Yes, in moderation. Plan it into your meal and monitor your sugar.
Q. What’s the normal blood sugar range?**
Fasting: 80–130 mg/dL
After meals: <180 mg/dL
Q. Is rice bad for diabetes?**
Not necessarily. Choose brown or hand-pounded rice in small portions.
Q. What is the A1C test?**
It shows your average blood sugar over 3 months. Aim for <7%.
Call-to-Action (CTA) Options:
**“Have questions about managing diabetes? Share your thoughts or ask in the comments,let’s support each other!”**