Hypertension management protocol helps you control high blood pressure with simple lifestyle changes, medications, and regular monitoring.
Introduction:
High blood pressure, or hypertension, is a silent but dangerous condition that affects millions of people worldwide. Often, it shows no symptoms until it has already damaged vital organs.
That is why medical professionals call it a “silent killer”. Early detection, effective management, and prevention of major complications such as heart attack, stroke, kidney failure, and vision loss are the main objectives of a hypertension management protocol.
We will examine the diagnosis, treatment, and monitoring of hypertension in this comprehensive guide. In addition, we will discuss medical treatment options, lifestyle strategies, and long-term control tips.

Prevalence of Hypertension in the World-
Whenever we concentrate on the issue of how much it is a silent killer, then we should focus on the prevalence of this disease on a global basis. As per data from the World Health Organisation (WHO) and other reliable sources, it is estimated that around 1.5 billion people will have hypertension in 2025. This is a considerable rise from the estimated 972 million people living with hypertension in the year 2000.
Attributable Deaths:
In every year hypertension majorly contributed so many risk factors for the emergence of the different types of Non-Communicable Diseases (NCD), especially cardiovascular diseases and stroke, to a significant number of deaths globally. The report has stated that 7.5 million deaths occur annually from hypertension.
Prevalence of Hypertension in India—
It is very difficult to find out about the exact figure of prevalence on that particular issue in India for 2025. As per data from the National Family Health Survey (NFHS), a report has been explored through the initiative named the “75/25” initiative; near about 75 million people are living with hypertension and diabetes under standard care, and the most remarkable thing is that it is progressing.
According to older data from the National Institutes of Health (NIH), as of March 5, 2025, there are 42.01 million people accessing the treatment of hypertension, projecting 22.9% for men and 23.6% for women, which has been raised from 2005 to 2025. The actual figure may be more due to the raising of different non-communicable diseases and increasing the awareness and increasing the screening efforts.
Understanding Hypertension
Blood pressure is the force of blood pushing against the walls of the arteries. It is measured in millimeters of mercury (mmHg) and recorded as two numbers: systolic pressure (when the heart beats) over diastolic pressure (when the heart rests between beats).
Normal blood pressure: Less than 120/80 mmHg
Elevated blood pressure: 120–129/<80 mmHg
Stage 1 hypertension: 130–139/80–89 mmHg
Stage 2 hypertension: 140/90 mmHg or higher
If the reading is consistently high on multiple occasions, it is considered hypertension.

Evaluation Steps
1. BP Measurement
2. Lifestyle Check: Salt, smoking, alcohol, stress
3. Risk Factors: DM, CKD, CVD → Refer to tertiary care
Risk Factors
| Modifiable Risk Factors | Relatively Fixed Risk Factors |
| Current Smoking, Secondhand Smoking Diabetes Dyslipidemia Overweight / Obesity Physical inactivity / low fitness Unhealthy diet | CKD Family History Increased Age Male sex Low socioeconomic/educational status Obstructive sleep apnea Psychological Stress |
Basic Investigations
| Basic Laboratory Test | Fasting Blood Glucose Serum Creatinine with eGFR Urinalysis |
| 2nd Tier | Complete Blood Count Lipid Profile Serum Sodium, Potassium Urea, Creatinine Uric Acid Urinary Albumin to Creatinine Ratio Thyroid Profile ECG, Halter |
| 3rd Tier | Echocardiogram, Angiogram, CT-Angiogram |
BP Treatment Targets
- Age 18–65: SBP <130 (not <120)
- Age >65: SBP 130–139
- DBP for all: 70–79 mmHg
- Control value = SBP <140 and/or DBP <90
Hypertension Management Protocol:
Step 1: Accurate Diagnosis:
Navigating the problem of hypertension, proper comprehensive digenesis is the foundation of hypertension management protocol, this includes:
1. Multiple Measurements:
Blood pressure should be checked on at least two separate visits.
Use a validated blood pressure monitor.
Take the reading after the patient has been seated quietly for 5 minutes.
Avoid caffeine, smoking, or exercise 30 minutes before the test.
2. Ambulatory Blood Pressure Monitoring:
In some cases, doctors use 24-hour monitoring to confirm the diagnosis, especially if there is suspected “white coat hypertension” (high readings only in clinical settings and medical suprvison).

BP Control Summary
Screen ≥30 yrs
Accurate measurement
Lifestyle + Drugs = Control
Regular follow-up & timely referral
3. Identifying Secondary Causes:
Most of the primary cases of hypertension, there is no any definite cause, but some of other secondary co- morbid condition like kidney disease, hormonal disorders, or certain medications are responsible for hypertension.
Step 2: Risk Assessment:
After diagnosis, doctors assess cardiovascular risk by checking for:
Family history of heart disease
High cholesterol
Diabetes
Smoking habits
Obesity
Sedentary lifestyle
This helps decide how aggressive the treatment should be.
Step 3: Lifestyle Modifications:
Lifestyle changes are the first and most important step in controlling blood pressure. Even small improvements can have a big and sustainable impact.
3.1 Dietary Changes-
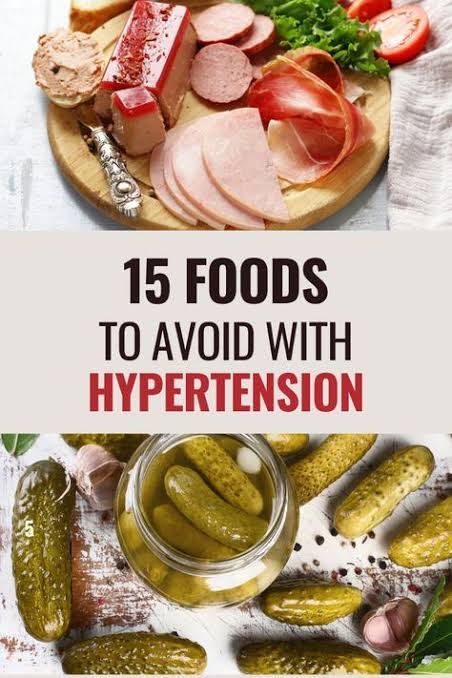
1. Salt <5 gm/day
2. DASH Diet
3. BMI 20–25
4. 30-min walk × 5 days
5. Stop tobacco/alcohol
6. Potassium supplements and enriched foods like bananas, spinach, and sweet potatoes help counter sodium effects.
7. Making a comprehensive diet plan, emphasizing fruits, vegetables, whole grains, lean protein, and low-fat dairy.
8. Intake of limited process Food: Packaged snacks, instant noodles, and processed meats have high hidden sodium.
9. Intake of Healthy Fats: Choose unsaturated fats from olive oil, nuts, and fish instead of saturated fats.

3.2 Weight Management
Overweight or trends of obesity lead to increased hypertension or CVD; it creates significant improvement for lowering blood pressure through losing 5-10% of body weight.
Through this approach the optimal goal is to achieve ideal body weight, but any weight loss is desirable. It is expected that 1 mmHg can be reduced in SBP for the loss of every 1 kg of body weight.
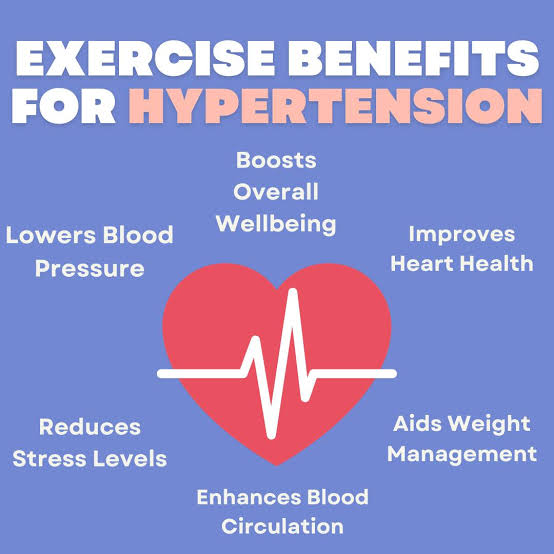
3.3 Physical Activity
In the research it has been explored that at least 150 minutes of moderate aerobic exercise per week is likely brisk walking (5-7 X/wk) (30-60 min/session), cycling, or swimming. Include muscle-strengthening activities twice a week, considering the algorithm, like gradual start-up at the start and cool-down at the end of each session.
Apart from that, under the supervision of any exercise professional, weight lifting and circuit training at least 2–3×/wk also play a very effective role in fostering aerobic exercise, and isometric resistance exercise, such as hand-grip training regimens, at least 3–4×/wk, also plays a vital role in the betterment of hypertension patients.
3.4 Alcohol Moderation
Limit alcohol (men: ≤2 standard drinks/d and women: ≤1 standard drink/d) to one drink per day for women and two for men. Excess alcohol can raise blood pressure.
3.5 Quitting Smoking
Smoking damages blood vessels and accelerates hypertension complications. Quitting is a critical step.
3.6 Stress Reduction
Stress is not good for health; moreover, chronic stress can increase the blood pressure temporally and foster the coping habits of gaining weight and drinking. In this regard, some lifestyle modifications like deep breathing, meditation and yoga can help to manage and control the blood pressure.
Step 4: Management through medication
Whenever lifestyle modification is not enough to bring down blood pressure, medication is the only effective way for the management of hypertension.
Typical classification of antihypertensive drugs
1. Diuretics
Applying this drug, the body can eliminate excess sodium and water, such as hydrochlorothiazide.
2. ACE Inhibitors
This type of medicine is applied for the prevention of blocking the hormones that lead to the creation of narrow blood vessels, which are responsible for hypertension, but applying this makes the blood vessels more relaxed. Such as the use of lisinopril.
3. Angiotensin II Receptor Blockers (ARBs)
This type of medication is applied for the same purpose as ACE inhibitors, but in this case it directly affectshormone blocking, such as the use of losartan.
Pharmacological Steps:
| Step-1 | ⤇ | Manotherapy Low risk grade one Hypetension or in very old (>80 year)frailer patient) | ⤇ | CCB/ACEI/ARB/THIAZIDE CCB is prefered | |
| Step-2 | ⤇ | Dual Cobination | ⤇ | CCB or Thiazide + ACEi or ARB | |
| Step-3 | ⤇ | Tripal Cobination | ⤇ | CCB + Thiazide + ACEi or ARB | |
| Step-4 | ⤇ | Resistant Hypertension | ⤇ | To add spironolactone orother diuretics or alpha or beta blockrs | Referral to tertiary Centre |
Drugs with Dosages and Side Effects
| Group | Drugs | Doses (mg/day) | Daily Frequency | Adverse Effects |
| First Line Drugs | ||||
| CCB (Calcium Channel Blockers) | Amlodipine Cilnidipine | 2.5 – 10 5 – 20 | 1 1 or 2 | Ankle edema, |
| ACEi (ACE Inhibitors) | Enalapril Ramipril | 5 – 40 2.5 – 20 | 1 or 2 1 or 2 | Angioedema, Cough, Hyperkalemia |
| ARB (Angiotensin Receptor Blockers | Losartan Olmesartan Telmisartan | 50 – 100 20 – 40 20 – 80 | 1 or 2 1 1 | Angioedema, Hyperkalemia |
| Thiazide Diuretics | Valsartan Hydrochlorothiazide Chlorthalidone | 80 – 320 12.5 – 25 6.25 – 25 | 1 1 1 | Hyponatremia, Hypokalemia |
| Second Line Drugs | ||||
| Loop Diuretics | Furosemide Torsemide | 20 – 80 5 – 40 | 2 1 | Hypokalemia |
| Aldosterone Antagonist | Spironolactone Eplerenone | 25 – 100 50-100 | 2 1 or2 | Hyperkalemia |
| Beta Blockers | Bisoprolol Metoprolol succinate Nebivolol Carvedilol Labetelol | 1.25 – 10 50- 200 2.5 – 20 12.5 – 50 100 – 800 | 1 1 1 2 2 | Bradycardia, Hypotension Contraindicated in Bronchial Asthma |
| Alpha-1 Blocker | Prazosin | 2 – 20 | 2 | 1st dose hypotension |
| Centrally Acting | Clonidine Methyldopa | – 0.8 250 – 500 | 2 | Rebound hypertension |
| Vasodilators | Hydralazine Minoxidil | 100-200 5 – 50 | 2-3 1-3 | Hypotension |
Special situation
• Hypertension with Diabetes Mellitus: Proteinuria should be looked for in patients with hypertension and diabetes. ACEi / ARB is the drug of choice if proteinuria is present.
• Hypertension with Chronic Kidney Disease:
– If the albumin-to-creatinine ratio is >300, ACEi/ARB should be the first line.
– Where eGFR is <30 or hyperkalemia is present, ACEi/ARB should be avoided.
– CCBs/diuretics should be the first-line drugs. Beta-blockers, alpha-blockers, or vasodilators may be considered as add-ons.
• Hypertension with Associated Cardiovascular Risk Factors:
Beta-blockers are the preferred first line in CVD. ACEi / ARB can be used. Statin therapy as per ASCVD score.
Gestational HTN
Step 1: Diagnosis & Classification
• BP 140–159/90–109 mmHg → Gestational Hypertension
• BP ≥160/110 mmHg → Severe Gestational Hypertension
• Hypertension + Proteinuria/End-organ damage = Pre-eclampsia + Seizures = Eclampsia
Step 2: Management Based on Severity
• If Mild Hypertension (BP 140–159/90–109 mmHg):
• First-Line Treatment:
• Methyldopa (250 mg TID) or
• Labetalol (100 mg BID) or
• Nifedipine SR (10 mg BID)
Supportive Care:
• Lifestyle modifications (low-salt diet, moderate activity)
• Monitor BP every 2 weeks
• Fetal monitoring (growth scan, Doppler, fetal movements)
Referral to Higher Center If:
• BP ≥160/110 mmHg
• Symptoms of preeclampsia (headache, vision changes, etc.)—refer with a loading dose of MagSulph
Gestational HTN
If Severe Hypertension (BP ≥160/110 mmHg):
- Immediate hospital admission (Secondary/Tertiary Care Level)
First-Line Treatment:
- IV Labetalol (20 mg bolus → Repeat every 10–30 min up to 300 mg) or
- Oral Nifedipine (10 mg every 30 min, max 40 mg/day)
Alternative Treatment:
- IV Hydralazine (5–10 mg slow IV every 20 min if BP remains high)
In PET settings give MgSO4 as per norm
Monitoring :
- BP every 15–30 min until controlled
- Urine protein, platelet count, liver function tests
- Fetal well-being (Doppler, CTG)
Referral to Tertiary Care If:
- No BP control despite treatment
- Signs of impending eclampsia
If Eclampsia (BP ≥160/110 + Seizures):
- Emergency ICU Admission
- Magnesium Sulfate (MgSO₄) Protocol:
- Loading dose: 4 g IV over 10 min + 5 g IM in each buttock
- Maintenance dose: 5 g IM on alternate buttock every 4 hr.ly for 24 hours after last seizure or, delivery whichever is later
BP Management:
- IV Labetalol or IV Hydralazine (as in severe HTN)
Delivery Plan:
- If ≥34 weeks: Induce labor or C-section
- If <34 weeks: Consider steroids for fetal lung maturity
Gestational HTN
| Healthcare Level | Mild Hypertension | Severe Hypertension | Eclampsia |
| Primary Care (PHC/CHC | Methyldopa, Labetalol | Referral if BP ≥160/110 | Referral, initiate MgSO₄ if available |
| Secondary Care (District Hospital) | Labetalol, Nifedipine | IV Labetalol, Hydralazine | Full MgSO₄ protocol, ICU admission |
| Tertiary Care (Medical College/Hospital) | Continue treatment | ICU monitoring, fetal assessment | Emergency delivery if necessary |
Step 4: Postpartum Management
• Monitor BP every 4–6 hours for 48 hours postpartum.
• Continue medication for 2 to 6 weeks with antihypertensives, like methyldopa, labetalol,
or nifedipine, which is most applicable.
• At the time of exclusively breastfeeding, safe medication can be applied through
Methyldopa, labetalol, and nifedipine: which is most effective?
• For the assessment of chronic hypertension of any postpartum mothers, BP
Should be followed up with a check at 6 weeks
Regular Monitoring and Follow-Up
It is essential to monitor the blood pressure on a regular basis for the patient with hypertension, because it is a long-term condition.
Home Monitoring:
To know the trends of blood pressure, the protocol recommends that hypertension patients monitor it regularly at home.
Clinic Visits:
In this case, follow-up visits should be done in a consistent manner, fostering the adjustment of medication and teasing out its side effects.
Blood Tests: Periodically done to monitor kidney function, cholesterol, and other risk factors.
AM/PM dosing if ≥2 drugs
First in 2 months, then every 6 months
Monitor side effects.
Reassess CV risks every 2 years.
4. Calcium Channel Blockers
Relax blood vessels and reduce heart workload. Example: Amlodipine.
5. Beta Blockers
Depending on the age, race, co-morbidity conditions and tolerance of side effects of patients, atenolol is used for reducing heart rate and outputs.
Step 6: Management of Coexisting Conditions
The occurrence of hypertension occurs along with other associated health conditions like:
Diabetes: The presence of a high level of sugar in the blood can damage arteries and create blood pressure.
High Cholesterol: The presence of high cholesterol creates the risk of atherosclerosis.
Chronic Kidney Disease: Both a cause and effect of hypertension.The management protocol should be addressed together for better management outcomes of the approach.
Step 7: Educating the Patient
The patient should be aware and educated on the following concerns:
Should know what the correct approach is for measurement of blood pressure at home.
Should be given more importance for taking medication on a regular basis.
Should be aware and educated about the warning signs of hypertensive crisis, like chest pain, severe headache, frequent changes of vision and shortness of breath.
Step 8: Protocols of Emergency
When a patient hasa blood pressure like above 180/120 mmHg, they should be hospitalised immediately for hospital care. In this hypertensive crisis situation intravenous medication is the only most effective approach for lowering blood pressure.
Long-Term Approach
Most of the people who are suffering from hypertension can lead healthy lives without major complications through proper management, early detection, consistent follow-up and sticking to the treatment plan.
Strictly follow the Practical Daily Checklist for the Hypertension Management protocol.
1. Taking measurement of blood pressure and preparing a checklistevery day at the same time.
2. Eat at least five servings of fruits and vegetables.
3. Avoiding taking extra salt at the time of food intake.
4. Get at least 30 minutes of physical activity.
5. Take prescribed medication without skipping doses.
6. Sleep 7–8 hours nightly.
7. Avoid tobacco and limit alcohol.
8. Manage stress through relaxation techniques.
RESISTANT HYPERTENSION:
One of the largest risks to cardiovascular health in the world is still high blood pressure. Our knowledge of the definition, diagnosis, and treatment of hypertension has continued to advance over time.
The 2017 ACC/AHA guideline, which reduced the general blood pressure (BP) treatment goal to less than 130/80 mm Hg, was one of the most significant changes in this area.
Additionally, the definition of resistant hypertension (RH) was altered, leading to a more accurate understanding and increased recognition of the condition.
In this regard, the American Heart Association (AHA) has clarified the new definition of resistant hypertension in a scientific statement published in the year 2018.
This guideline states that RH is diagnosed when a patient takes three different classes of antihypertensive medications at maximum or maximally tolerated doses, but their blood pressure still exceeds the target goal.
These typically consist of:
A calcium channel blocker with a long half-life
An ACE inhibitor or an angiotensin receptor blocker is a renin-angiotensin system blocker.
A diuretic
The RH category also includes patients who require four or more antihypertensive medications from various classes in order to achieve their blood pressure target.
The Value of Not Including Pseudo-Resistance:
The requirement to rule out “pseudo-resistance” before classifying a patient as resistant was a significant modification to the 2018 definition.
The white coat effect, inaccurate blood pressure readings, and noncompliance with recommended treatment are examples of pseudo-resistance.
Since many patients who seem resistant might not be taking their medications regularly or may not be receiving accurate measurements, this step is essential.
Before confirming a diagnosis of resistant hypertension, pseudo-resistance should be ruled out, according to the American Heart Association and the European Society of Cardiology/European Society of Hypertension (ESC/ESH).
How Home and Ambulatory BP Monitoring Work :
Although office blood pressure is still the accepted reference, guidelines now advise using methods outside of the office to confirm readings.
The result of more accuracy of measurement of blood pressure for the person with hypertension is obtained using home bolus blood pressure measurement and ambulatory blood pressure monitoring (ABPM).
A study reveals that the lower threshold of 130/80 mm Hg is found in office blood pressure, whereas<125/75 mm Hg has been found in ABPM within 24 hours.
The finding of the research is that cooperatively clinic-based measurement and ambulatory blood pressure measurement (ABPM) have a close relationship with long-term cardiovascular and renal outcomes.
During treatment, follow-up ABPM is particularly crucial. Ambulatory readings during treatment were found to be more strongly associated with adverse cardiovascular events and mortality than baseline measurements in a study that included over 1,700 patients with resistant hypertension.
Accordingly, serial ABPM can help guide better treatment adjustments and enhance risk prediction.
The prevalence of resistant hypertension and its prognosis:
Many experts anticipated a sharp rise in the prevalence of RH when the 2017 ACC/AHA guideline lowered the BP cutoff to <130/80 mm Hg.
However, U.S. population studies only predicted a slight increase, roughly 2%, from 17.7% to 19.7%.
RH carries a higher risk of heart disease, stroke, kidney damage, and mortality than non-resistant hypertension, so even though prevalence did not increase as much as anticipated, it is still a significant clinical issue.
This worry was validated by a sizable Korean cohort study with 2,000 patients. RH was associated with increased risks of major cardiovascular events, including heart attack, stroke, heart failure, and cardiovascular death, as well as adverse kidney outcomes, even after patients with the white coat effect were excluded.
It’s interesting to note that this study demonstrated that risk could be predicted with both the old and new definitions of RH, confirming the updated guidelines’ robustness.
Aortic Stiffness’s Function:
Aortic stiffness, as determined by carotid-femoral pulse wave velocity, is one new factor in RH.
Increased aortic stiffness was linked to a two- to three-times higher risk of cardiovascular events and mortality, according to a study of almost 900 patients with resistant hypertension.
As a result, aortic stiffness may be a sign of worse outcomes in addition to being a result of chronically high blood pressure.
In light of these results, adding pulse wave velocity measurements to the resistant hypertension workup could enhance risk assessment and treatment choices.
Checking for Hypertension’s Secondary Causes:
In accordance with the 2018 AHA scientific statement and the 2017 ACC/AHA guideline, all RH patients are considered for screening for secondary causes.
Among the resistant hypertension patients, about 20% suffer from primary aldosteronism, which promotes an increase in the prevalent secondary causes.
Studies show that only 1.6–2.1% of RH patients have primary aldosteronism, which is regrettably still a very low screening rate.
Since primary aldosteronism has effective treatment options and carries significant cardiovascular and renal risks, this is a lost opportunity.
While mineralocorticoid receptor antagonists (MRAs) work well for bilateral cases, surgery (adrenalectomy) may be curative for unilateral disease.
In this patient population, increasing screening rates may greatly lower long-term complications.
Handling Resistant Hypertension Step-by-Step:
A new step-by-step method for treating resistant hypertension was suggested in the 2018 AHA Scientific Statement:
Optimise the first three-drug regimen.
Ascertain the right medication selection, maximum tolerated dosages, and suitable dosing schedules.
When required, switch diuretics. A thiazide-like diuretic, like indapamide or chlorthalidone, has stronger and longer-lasting effects than hydrochlorothiazide. Include an antagonist of the mineralocorticoid receptor (MRA).
The recommended fourth-line medications are eplerenone or spironolactone. The superiority of spironolactone over other adjuvant agents was validated by the PATHWAY-2 trial.
Address issues unique to drugs:
Because spironolactone inhibits androgen receptors, it may have hormonal side effects.
Eplerenone needs to be taken twice daily due to its lower potency.
With fewer adverse effects and a decreased risk of hyperkalaemia, newer nonsteroidal MRAs like esaxerenone and finerenone show promise.
The AMBER trial showed that spironolactone can be used in conjunction with potassium-binding medications such as patiromer to lower the risk of hyperkalaemia in patients with chronic kidney disease.
Intense Reduction of Blood Pressure in RH:
The SPRINT trial demonstrated that intensive blood pressure reduction improves cardiovascular outcomes more than standard treatment; thus, it is very important evidence of this study.
This emphasises how crucial it is to aim for aggressive blood pressure targets when tolerated instead of settling for modest control.
Important Takeaways:
The recent definition of resistant hypertension is <130/80 mm Hg.
Prior to diagnosis, pseudo-resistance needs to be ruled out.
Accurate assessment requires both home blood pressure monitoring and ABPM.
Compared to non-resistant hypertension, RH carries greater risks for the kidneys and heart.
Poor outcomes can be independently predicted by aortic stiffness.
In RH, primary aldosteronism is prevalent but not well recognised.
Results are improved by stepwise treatment optimisation, which includes MRAs and more recent agents.
We can protect or reduce the frequency of suffering from any cardiovascular diseases through following recommended steps for reducing the aggressive blood pressure reduction.
In this context additionally, we should focus on following the assessment and methodical treatment protocol of the persisting blood pressure issue because resistant hypertension is directly responsible for the occurrence of elevated cardiovascular and renal risk.
Final Thoughts
The plan for hypertension management protocol is not applicable for universal.
The protocol has been formulated on the basis of patients’ conditions, associated risk factors, and lifestyle. The basic components of the protocol comprise combining lifestyle modifications, proper medical treatment, proper guidance and education for patients and, after all, medical treatment. So protocol gives the best chance for long-term control.
Through following all instructions of this protocol, you can protect your blood pressure, heart, brain, kidneys and overall wellbeing of health.
Hypertension in Teens: Why Early Awareness Is Crucial
It is a very crucial issue to raise awareness about the hypertension in the adolescent phase today, because the practice of a sedentary lifestyle persists in future life and promotes the creation of serious health issues like cardiovascular disease, kidney disease, and stroke.
As for the prevalence of hypertension among adolescents, a large-scale study in India found that 35.1% of adolescents aged 10–12 and 5.1% of those aged 13+ exhibit high blood pressure, often linked with obesity, high fasting glucose, and elevated LDL cholesterol.
A rising trend among youth globally, it has been found recent data from the U.S. shows 8.7% of young people (ages 8–19) have elevated blood pressure and 5.4%** meet hypertension criteria, highlighting a growing, often overlooked issue.
Early screening and proper management through lifestyle modification and the right way of medical intervention foster decreasing the probability of the development of complicated issues for adolescents in young stages.
Additionally, it can be said that for reducing the onset of complications in the early stage, adolescence is the only phase of life where modification can be done at the right time for prevention.
Here are some points that have been expressed for awareness regarding this issue:
· Hypertension Tracking:
Different intensive research studies express that the trends of hypertension in the adolescent stage persist in adulthood if he/she has not adopted any comprehensive approach for its modification.
· Early Onset of Complications:
The prevalence data of hypertension in adolescents indicates that there is a tendency forchance to grow cardiovascular diseases, such as heart disease and stroke, left ventricular hypertrophy, increased arterial stiffness, and increased carotid intima-medial thickness earlier in life.
Being unaware about this issue in most of the adolescents, myocardial infarction, congestive heart failure, and kidney failure are found in young adults.
· Behaviour Modification:
Adolescence is the golden period of human life because it is the only period of life where lifestyle can be changed, and as a result, it is very effective for the prevention of early infection with hypertension and other associated risk factors of life.
· Preventative Measures:
Early screening and comprehensive management of hypertension through intake of a proper nutritional diet, regular exercise, control of BMI, and proper medical intervention (if needed) can promote prevention or delay the onset of health issues.
Conclusions
Today hypertension is the leading risk factor for cardiovascular diseases (CVD) and mortality in the world and increases its severity for the person with comorbid conditions like diabetes or other associated non-communicable diseases. The research process is ensuing, and several new findings have emerged, approaching for better detection, prevention and management of hypertension.This innovative approach leads to increased awareness among the general population and makes them more likely to prevent CVD (heart attacks, strokes, and uncontrolled hypertension) and reduces morbidity (diabetes and kidney failure) and mortality in this regard in the future.
10 ways to control high blood pressure without medication
Disclaimer:
This content has not any intention to misconduct any steps of treatment guidance towards the patient living with hypertension; all the data and treatment protocol have been explored according to different medical professionals, but it is the recommendation to all the audience to follow the medical advice from your medical practitioner accordingly, because your degree of disease is very specific.
FAQs:
1. What is the Hypertension Management Protocol?
The hypertension management protocol itself is a comprehensive approach of step-by-step clinical guidelines and is fully designed for fostering help to high blood pressure patients through lifestyle modification, medication and exclusive monitoring and follow-up.
2. Why is the Hypertension Management Protocol important?
It is a very important and unique approach because it is a very structural and multilayered service used to reduce high blood pressure, reduce the risk of cardiovascular diseases (like heart disease, stroke, etc.) and improve overall quality of life.
3. Who should follow the Hypertension Management Protocol?
Anybody who has been screened as having high blood pressure, particularly those who are over 30 years old andlike diabetes, obesity, kidney failure or renal failure and a familial history of hypertension, should follow this protocol.
4. How does the Hypertension Management Protocol help in controlling blood pressure?
This particular protocol is a combined approach, like lifestyle modification, planned diet intake, exercise, proper medication, and regular follow-up, for ensuring blood pressure remains in a safe range.
5. What lifestyle changes are included in the Hypertension Management Protocol?
Through this particular protocol, lifestyle modification occurs through –
Reducing salt intake
The diet plan should cover the maximum intake of fruit and vegetables.
Regular follow-up of Body Mass Index (BMI)
Engaging in exercise on a regular basis
Alcohol consumption should be confined to a limited level.
Quitting smoking.
6. Can diet alone control hypertension under this protocol?
The patients of hypertension belong in the mild category; a comprehensive diet plan and lifestyle modification are enough to navigate this situation. But most moderate and severe situations should require a structural medication protocol.
7. What role does medication play in the hypertension management protocol?
In this concern, medication is required whenever lifestyle changes are not sufficient to control this situation. To overcome this situation, the basic medicines are applied, like calcium channel blockers, ACE inhibitors, beta blockers and diuretics.
8. How often should blood pressure be checked under this protocol?
In the beginning, blood pressure should be measured at least once every two weeks. Whenever it is achieved, then the frequency of blood reassuring should be followed as per the doctor’s advice.
9. What is the target blood pressure in the Hypertension Management Protocol?
The targeted blood pressure for adults is generally below 140/90 mmHg, and for the case of diabetes or kidney disease patients, below 130/80 mmHg.
10. Can the Hypertension Management Protocol prevent complications?
Obviously yes, if a hypertension patient followed this prescribed protocol correctly, then he/she could reduce the severity of the risk of stroke, loss of vision, heart attack, and kidney failure.
11. Is the hypertension management protocol the same for everyone?
No, the management protocol is designed in accordance with the patient’s age, lifestyle history, medical history, and response to treatment.
12. Are home blood pressure monitors recommended in this protocol?
Yes, in these cases, the protocol advisesthe patients to track their frequency of ups and downs of blood pressure by monitoring it in-house on a regular basis, and the track record alerts the patient to contact a medical practitioner whenever it is needed.
13. How often should patients visit the doctor as per protocol?
Generally, every one or three months, they visit their doctors in the initial stage, but frequency should be followed as per the medical advice of the doctor.